.jpg)
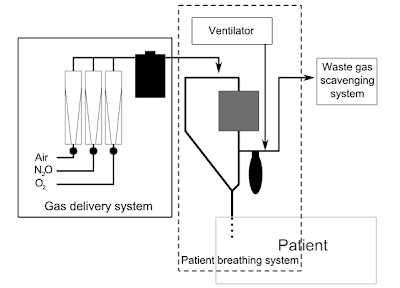
The anaesthetic machine (or anesthesia machine in America) is used by anesthesiologists to support the administration of anaesthesia. The most common type of anaesthetic machine in use in the developed world is the continuous-flow anaesthetic machine, which is designed to provide an accurate and continuous supply of medical gases (such as oxygen and nitrous oxide), mixed with an accurate concentration of anaesthetic vapour (such as isoflurane), and deliver this to the patient at a safe pressure and flow. Modern machines incorporate a ventilator, suction unit, and patient-monitoring devices.
The original concept was invented by the British anaesthetist H.E.G. Boyle in 1917. Prior to this time, anaesthetists often carried all their equipment with them, but the development of heavy, bulky cylinder storage and increasingly elaborate airway equipment meant that this was no longer practical for most circumstances. The anaesthetic machine is usually mounted on anti-static wheels for convenient transportation.
Simpler anaesthetic apparatus may be used in special circumstances, such as the TriService Apparatus, a simplified anaesthesia delivery system invented for the British armed forces, which is light and portable and may be used effectively even when no medical gases are available. This device has unidirectional valves which suck in ambient air which can be enriched with oxygen from a cylinder,with the help of a set of bellows. A large number of draw-over type of anaesthesia devices are still in use in India for administering an air-ether mixture to the patient, which can be enriched with oxygen. But the advent of the cautery has sounded the death knell to this contraption, due to the explosion hazard.
Many of the early innovations in U.S. anaesthetic equipment, including the closed circuit carbon-dioxide absorber (aka: the Guedel-Foregger Midget) and diffusion of such equipment to anaesthetists within the United States can be attributed to Dr. Richard von Foregger and The Foregger Company.Based on experience gained from analysis of mishaps, the modern anaesthetic machine incorporates several safety devices, including:.jpg)
an oxygen failure alarm (also known as 'Oxygen Failure Warning Device' or OFWD). In older machines this was a pneumatic device called a Ritchie whistle. Newer machines have an electronic sensor. nitrous cut-off: the flow of medical nitrous-oxide is dependent on oxygen pressure. This is done at the regulator level. In essence, the nitrous-oxide regulator is a 'slave' of the oxygen regulator. hypoxic-mixture alarms (hypoxy guards or ratio controllers) to prevent gas mixtures which contain less than 21% oxygen being delivered to the patient. In modern machines it is impossible to deliver 100% nitrous oxide (or any hypoxic mixture) to the patient to breathe. Oxygen is automatically added to the fresh gas flow even if the anaesthetist should attempt to deliver 100% nitrous oxide. Ratio controllers usually operate on the penumatic principle or are chain linked. Both are located on the rotameter assembly, unless electronically controlled. ventilator alarms, which warn of disconnection or high airway pressures interlocks between the vaporisers preventing inadvertent administration of more than one volatile agent concurrently alarms on all the above physiological monitors the Pin Index Safety System prevents cylinders being accidentally connected to the wrong yoke the NIST (Non-Interchangeable Screw Thread) system for pipeline gases, which prevents piped gases from the wall being accidentally connected to the wrong inlet on the machine pipeline gas hoses have non-interchangeable Schrader valve connectors, which prevents hoses being accidentally plugged into the wrong wall socket The functions of the machine should be checked at the beginning of every operating list in a "cockpit-drill". Machines and associated equipment must be maintained and serviced regularly.
Older machines may lack some of the safety features and refinements present on newer machines. However, they were designed to be operated without mains electricity, using compressed gas power for the ventilator and suction apparatus. Modern machines often have battery backup, but may fail when this becomes depleted.
The modern anaesthetic machine still retains all the key working principles of the Boyle's machine (a British Oxygen Company trade name) in honour of the British anaesthetist H.E.G. Boyle (1875-1941). In India, however, the trade name 'Boyle' is registered with Boyle HealthCare Pvt. Ltd., Indore MP.
A two-person (Operating Theatre Practitioner and anaesthetist) pre-use check of the anaesthetic machine is recommended before every single case and has been shown to decrease the risk of 24-hour severe postoperative morbidity and mortality (Arbous et al Anesthesiology 2005). Various regulatory and professional bodies have formulated checklists for different countries - A free transparent reality simulation of the checklist recommended by the United States Food & Drug Administration is available from the Virtual Anesthesia Machine web site ( see below) after registration which is also free.A modern machine typically includes the following components:
connections to piped hospital oxygen, medical air, and nitrous oxide. Pipeline pressure from the hospital medical gas system (wall outlet) should be around 400 kPa (60 psi; 4 atmospheres). reserve gas cylinders of oxygen, air, and nitrous oxide attached via a specific yoke with a Bodok seal. Older machines may have cylinder yokes and flow meters for carbon dioxide and cyclopropane. Many newer machines only have oxygen reserve cylinders. The regulators for the cylinders are set at 300 kPa (45 psi; 3 atmospheres). If the cylinders are left on and the machine is plugged into the wall outlet, gas from the wall supply will be used preferentially, since it is at a higher pressure. In situations where pipeline gases are not available, machines may safely be used from cylinders alone, provided fresh cylinders are available. a high-flow oxygen flush which provides pure oxygen at 30 litres/minute pressure gauges, regulators and 'pop-off' valves, to protect the machine components and patient from high-pressure gases (referred to as 'barotrauma'). flow meters (rotameters) for oxygen, air, and nitrous oxide, which are used by the anaesthesiologist to provide accurate mixtures of medical gases to the patient. Flow meters are typically pneumatic, but increasingly electromagnetic digital flow meters are being used. one or more anaesthetic vaporisers to accurately add volatile anaesthetics to the fresh gas flow a ventilator physiological monitors to monitor the patient's heart rate, ECG, non-invasive blood pressure and oxygen saturation (additional monitors are generally available to monitor end-tidal CO2, temperature, arterial blood pressure central venous pressure, etc.). In addition, the composition of the gases delivered to the patient (and breathed out) is monitored continuously. breathing circuits, most commonly a circle attachment, or a Bain's breathing system, which are breathing hoses connected to a anaesthesia face mask a heat and moisture exchanger (HME) with or without bacteria-viral filter (HMEF). scavenging system to remove expired anaesthetic gases from the operating room. Scavenged gases are usually vented to the atmosphere. suction apparatus There is generally a small work bench built into the machine where airway management equipment is kept within ready reach of the anaesthetist. source : wikipedia.org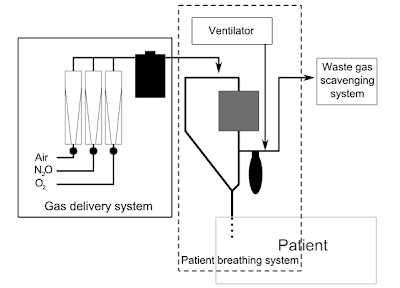
The original concept was invented by the British anaesthetist H.E.G. Boyle in 1917. Prior to this time, anaesthetists often carried all their equipment with them, but the development of heavy, bulky cylinder storage and increasingly elaborate airway equipment meant that this was no longer practical for most circumstances. The anaesthetic machine is usually mounted on anti-static wheels for convenient transportation.
Simpler anaesthetic apparatus may be used in special circumstances, such as the TriService Apparatus, a simplified anaesthesia delivery system invented for the British armed forces, which is light and portable and may be used effectively even when no medical gases are available. This device has unidirectional valves which suck in ambient air which can be enriched with oxygen from a cylinder,with the help of a set of bellows. A large number of draw-over type of anaesthesia devices are still in use in India for administering an air-ether mixture to the patient, which can be enriched with oxygen. But the advent of the cautery has sounded the death knell to this contraption, due to the explosion hazard.
Many of the early innovations in U.S. anaesthetic equipment, including the closed circuit carbon-dioxide absorber (aka: the Guedel-Foregger Midget) and diffusion of such equipment to anaesthetists within the United States can be attributed to Dr. Richard von Foregger and The Foregger Company.Based on experience gained from analysis of mishaps, the modern anaesthetic machine incorporates several safety devices, including:
.jpg)
an oxygen failure alarm (also known as 'Oxygen Failure Warning Device' or OFWD). In older machines this was a pneumatic device called a Ritchie whistle. Newer machines have an electronic sensor. nitrous cut-off: the flow of medical nitrous-oxide is dependent on oxygen pressure. This is done at the regulator level. In essence, the nitrous-oxide regulator is a 'slave' of the oxygen regulator. hypoxic-mixture alarms (hypoxy guards or ratio controllers) to prevent gas mixtures which contain less than 21% oxygen being delivered to the patient. In modern machines it is impossible to deliver 100% nitrous oxide (or any hypoxic mixture) to the patient to breathe. Oxygen is automatically added to the fresh gas flow even if the anaesthetist should attempt to deliver 100% nitrous oxide. Ratio controllers usually operate on the penumatic principle or are chain linked. Both are located on the rotameter assembly, unless electronically controlled. ventilator alarms, which warn of disconnection or high airway pressures interlocks between the vaporisers preventing inadvertent administration of more than one volatile agent concurrently alarms on all the above physiological monitors the Pin Index Safety System prevents cylinders being accidentally connected to the wrong yoke the NIST (Non-Interchangeable Screw Thread) system for pipeline gases, which prevents piped gases from the wall being accidentally connected to the wrong inlet on the machine pipeline gas hoses have non-interchangeable Schrader valve connectors, which prevents hoses being accidentally plugged into the wrong wall socket The functions of the machine should be checked at the beginning of every operating list in a "cockpit-drill". Machines and associated equipment must be maintained and serviced regularly.
Older machines may lack some of the safety features and refinements present on newer machines. However, they were designed to be operated without mains electricity, using compressed gas power for the ventilator and suction apparatus. Modern machines often have battery backup, but may fail when this becomes depleted.
The modern anaesthetic machine still retains all the key working principles of the Boyle's machine (a British Oxygen Company trade name) in honour of the British anaesthetist H.E.G. Boyle (1875-1941). In India, however, the trade name 'Boyle' is registered with Boyle HealthCare Pvt. Ltd., Indore MP.
A two-person (Operating Theatre Practitioner and anaesthetist) pre-use check of the anaesthetic machine is recommended before every single case and has been shown to decrease the risk of 24-hour severe postoperative morbidity and mortality (Arbous et al Anesthesiology 2005). Various regulatory and professional bodies have formulated checklists for different countries - A free transparent reality simulation of the checklist recommended by the United States Food & Drug Administration is available from the Virtual Anesthesia Machine web site ( see below) after registration which is also free.A modern machine typically includes the following components:
connections to piped hospital oxygen, medical air, and nitrous oxide. Pipeline pressure from the hospital medical gas system (wall outlet) should be around 400 kPa (60 psi; 4 atmospheres). reserve gas cylinders of oxygen, air, and nitrous oxide attached via a specific yoke with a Bodok seal. Older machines may have cylinder yokes and flow meters for carbon dioxide and cyclopropane. Many newer machines only have oxygen reserve cylinders. The regulators for the cylinders are set at 300 kPa (45 psi; 3 atmospheres). If the cylinders are left on and the machine is plugged into the wall outlet, gas from the wall supply will be used preferentially, since it is at a higher pressure. In situations where pipeline gases are not available, machines may safely be used from cylinders alone, provided fresh cylinders are available. a high-flow oxygen flush which provides pure oxygen at 30 litres/minute pressure gauges, regulators and 'pop-off' valves, to protect the machine components and patient from high-pressure gases (referred to as 'barotrauma'). flow meters (rotameters) for oxygen, air, and nitrous oxide, which are used by the anaesthesiologist to provide accurate mixtures of medical gases to the patient. Flow meters are typically pneumatic, but increasingly electromagnetic digital flow meters are being used. one or more anaesthetic vaporisers to accurately add volatile anaesthetics to the fresh gas flow a ventilator physiological monitors to monitor the patient's heart rate, ECG, non-invasive blood pressure and oxygen saturation (additional monitors are generally available to monitor end-tidal CO2, temperature, arterial blood pressure central venous pressure, etc.). In addition, the composition of the gases delivered to the patient (and breathed out) is monitored continuously. breathing circuits, most commonly a circle attachment, or a Bain's breathing system, which are breathing hoses connected to a anaesthesia face mask a heat and moisture exchanger (HME) with or without bacteria-viral filter (HMEF). scavenging system to remove expired anaesthetic gases from the operating room. Scavenged gases are usually vented to the atmosphere. suction apparatus There is generally a small work bench built into the machine where airway management equipment is kept within ready reach of the anaesthetist. source : wikipedia.org